TABLE OF CONTENTS
01 What is gluten?
02 Why is gluten bad for some people?
03 Coeliac disease: an autoimmune reaction to gluten
04 Gluten sensitivity: when gluten causes symptoms but there is no coeliac disease
05 Typical nutritional deficiencies in gluten intolerance
06 Irritable bowel syndrome, wheat allergy and other causes
07 FODMAPs: a common confusion with gluten intolerance
08 Regeneration of the intestinal mucosa
09 Which foods contain gluten?
10 Conclusion: Should you avoid gluten?
Celiac disease, gluten sensitivity, typical nutritional deficiencies and foods you should avoid.
Gluten in food is very controversial these days. One in ten Germans already does without it in whole or in part. Many experts claim that it is safe for people who do not have celiac disease.
However, there are health experts who believe gluten is harmful to the majority of people. At Ogaenics, we also make sure that our natural vitamin and mineral supplements are gluten-free as a matter of principle. This article explains what gluten is and how it can affect health.
What is gluten?
Gluten are proteins found in grains such as wheat, rye, spelt and barley. Of the grains containing gluten, wheat is by far the most commonly consumed. The two main proteins in gluten are glutenin and gliadin. Gliadin is responsible for most of the negative health effects(1, 2) .
When flour is mixed with water, the gluten proteins form a sticky network that has a glue-like consistency. This makes dough elastic and allows bread to rise during baking. It also provides a texture that is easy to chew(3, 4).

Why is gluten bad for some people?
Most people tolerate gluten well. However, it can cause problems for people with certain health limitations. These include celiac disease, gluten intolerance, wheat allergy and some other diseases(5, 6).
Celiac disease: an autoimmune reaction to gluten
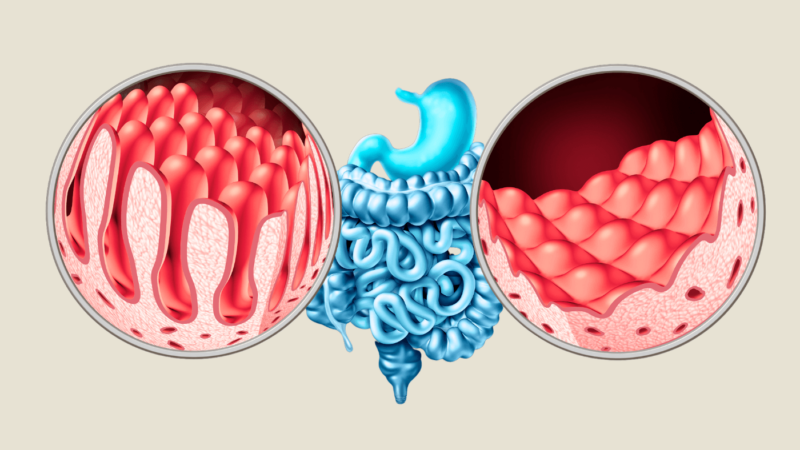
Coeliac disease is the most severe form of gluten intolerance and affects around 1% of the European population, in Germany around 0.4% of women and 0.2% of men(7,18)). It is an autoimmune disease in which the consumption of gluten triggers the immune system to attack the intestinal mucosa. This process leads to inflammation and damage to the villi of the small intestine, the hair-like structures responsible for the absorption of nutrients.
Symptoms of coeliac disease
Symptoms vary greatly from person to person and can affect both the digestive tract and other bodily functions.( 9) Common symptoms include:
- Abdominal pain, flatulence and diarrhea
- Chronic fatigue
- Weight loss
- Headache
- Depression
- Skin rashes (dermatitis herpetiformis)
- foul-smelling feces
- Growth disorders in children
Some sufferers also have so-called “silent” coeliac disease, where there are no obvious symptoms even though the intestinal mucosa is damaged.
Diagnosis of coeliac disease
The diagnosis usually involves two steps:
- Blood tests: The tTG-IgA test (tissue transglutaminase antibody) is the most common test to identify coeliac disease. A positive result indicates an immune reaction.
- Small intestine biopsy: If the blood test is positive, a biopsy is performed to confirm villous atrophy (damage to the villi of the small intestine).
It is important to continue consuming gluten before the diagnosis, as a gluten-free diet can falsify the test results.
Long-term treatment of coeliac disease
The only treatment option for coeliac disease is a strict, lifelong gluten-free diet. This reduces inflammation and allows the intestinal mucosa to regenerate. Nevertheless, it can take several months to years for the intestinal mucosa to heal completely.

Gluten sensitivity – also known as non-celiac gluten intolerance – is a condition in which people react to the consumption of gluten with symptoms similar to those of celiac disease(10). These include:
- Abdominal pain
- Flatulence
- Diarrhea or constipation
- Fatigue
- Headache
- Concentration problems
Unlike coeliac disease, however, gluten sensitivity does not lead to damage to the intestinal mucosa and no specific antibodies are detectable. The diagnosis is therefore made by ruling out other diseases such as coeliac disease or wheat allergy and by observing whether a gluten-free diet improves the symptoms(10).
How many people are affected?
The exact frequency of gluten sensitivity is difficult to determine. Scientific estimates vary widely and range from 0.5% to 13% of the population. This discrepancy is partly due to the fact that gluten sensitivity has no standardized diagnostic criteria and is often self-diagnosed(11, 12, 13, 14).
However, some experts believe that this is a misinterpretation. One study examined almost 400 people with self-diagnosed gluten intolerance and checked whether a gluten-free diet led to an improvement(17). The results showed that of the 400 people, only 26 people had celiac disease. Two had a wheat allergy and 27 were diagnosed as gluten-sensitive.
This means that of the 400 people who considered themselves to be gluten intolerant, only 14.5 percent actually had a problem with gluten. Or put another way, 85.5 percent had no gluten problem.
Neurological effects
While gluten sensitivity is primarily associated with digestive problems, new research shows that it could also cause neurological symptoms such as concentration problems and headaches. In some cases, evidence even points to possible damage to the brain. This research is still in its infancy, but it shows that gluten sensitivity could have effects beyond the gut(15).
Typical nutritional deficiencies with gluten intolerance
People with gluten intolerance, especially coeliac disease, often suffer from nutrient deficiencies, as the damaged intestinal mucosa impairs the absorption of vitamins and minerals or a gluten-free diet inevitably leads to nutrient deficiencies. Studies show that those affected often have deficiencies in iron, vitamin D and B vitamins, which in turn can lead to symptoms such as fatigue, anemia and a weakened immune system(16, 17).
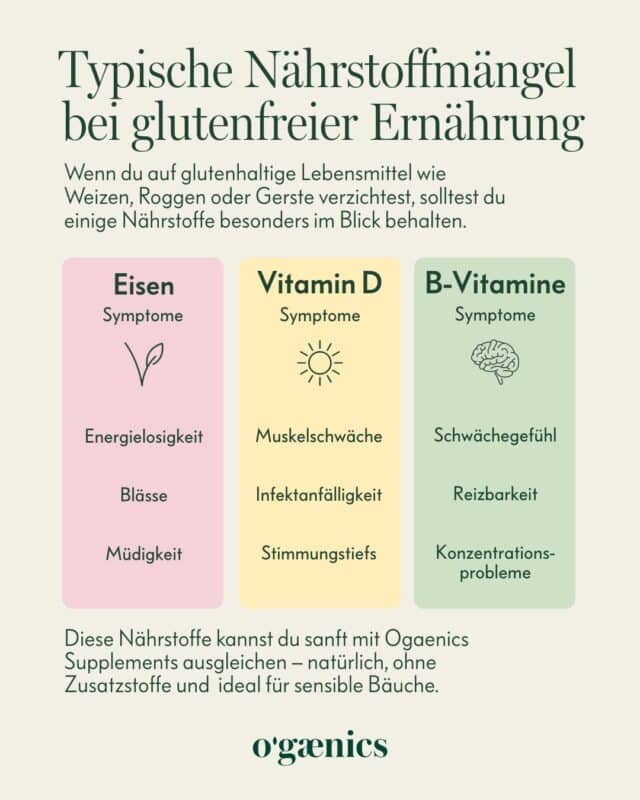
Iron deficiency
Iron deficiency is particularly common in coeliac disease patients and is one of the earliest diagnostic indicators of the disease. A strict gluten-free diet is required to effectively support the iron balance. Normalization of the anemic state usually occurs after at least 6 months of diet, but it may take up to 2 years to replenish iron stores. ( 18)
A highly bioavailable herbal supplement, such as Feed Your Blood from Ogaenics, can be useful in this phase. It is a blood formation complex specially designed for iron deficiency with potent doses of iron from organic curry leaves, combined with vitamin C for optimal absorption plus the co-factors for blood formation: active B12 and folate from organic plants.
Vitamin D deficiency
A lack of vitamin D, which is important for bone health and the immune system, is also common in coeliac disease. This deficiency can interfere with calcium absorption and increase the risk of osteoporosis(19). With Hello Sunshine D3+K2, Ogaenics offers a high-quality vitamin D supplement based on organic lichen that promotes bone health and can support the regulation of inflammatory processes in the gut.
B vitamins
A gluten-free diet often restricts the intake of B vitamins, as many gluten-free cereal products contain fewer B vitamins. This is where the gluten-free B-Happy Organic Vitamin B Complex from Ogaenics can help, as it provides all eight essential B vitamins in a bioactive, organic form and thus supports energy and nerve function.
Irritable bowel syndrome, wheat allergy and other causes
Irritable bowel syndrome (IBS) is a common digestive disorder that causes symptoms such as abdominal pain, cramping, bloating and diarrhea. It is a chronic condition, but can be well managed through diet, lifestyle and stress management techniques.
👉 You can find out why stress plays such a big role for your gut – and how you can counteract it – in our article “What stress really does to your gut”.
Recent studies have also shown that vitamin D deficiency may be responsible for IBS. Interestingly, studies have also shown that some people with irritable bowel syndrome can benefit from a gluten-free diet(20, 21).
In about one percent of the population, a wheat allergy can also be the cause of digestive problems after consuming gluten(22). In addition, studies have shown that individuals with schizophrenia and autism may benefit from a gluten-free diet(20, 21, 22).
FODMAPs: A common confusion with gluten intolerance
The term FODMAP stands for “fermentable oligo-, disaccharides (lactose) and monosaccharides (fructose) and polyols”. These are sugar substitutes such as xylitol/birch sugar. Many people are unable to digest FODMAPs properly, which can cause various problems.
FODMAPs are fermented by bacteria in the large intestine. Gases are produced during fermentation. These are usually responsible for the intestinal complaints.(23, 24)
In fact, there is some evidence that people with “gluten intolerance” are actually sensitive not to gluten but to FODMAPs. A study of 37 people with self-reported gluten intolerance put the participants on a low-FODMAP diet. The result: the symptoms subsided. The participants were then given isolated gluten. This did not trigger her digestive complaints(25). This shows that FODMAPs are often the actual cause of suspected gluten intolerance.
Regeneration of the intestinal mucosa
A key aspect in the treatment of coeliac disease or gluten intolerance and other intestinal problems is supporting the regeneration of the damaged intestinal mucosa. A healthy intestinal barrier is essential to absorb nutrients and reduce inflammation. Studies suggest that probiotics and omega-3 fatty acids can play a key role here(26, 27).
Probiotics for the intestinal flora
The composition of the intestinal flora has a strong influence on the intestinal mucosa. Probiotics promote the balance of microbes in the gut and support the healing of the barrier (6). The Love Your Gut Daily Biotic Complex from Ogaenics contains 21 strains of bacteria and organic fiber that can specifically promote gut health and reduce symptoms such as bloating and diarrhea.
-
Bestseller
Love Your Gut
Bio Daily Biotic Complex Premium for the gut: 21 bacterial strains plus organic fiberab 39,90 €2.660,00 € / kg
Omega-3 fatty acids for anti-inflammation
Omega-3 fatty acids have anti-inflammatory properties and can help to regenerate the intestinal mucosa and reduce inflammatory processes in coeliac disease and gluten intolerance (26). The Oilalala Skin Omega Complex from Ogaenics provides these essential fatty acids in high-quality organic form, combined with vitamin A to support mucosal function.
What foods contain gluten?
The most common sources of gluten in the diet are wheat, spelt, rye, barley, bread, pasta, beer, cakes, cookies and pastries. Wheat is also added to many types of processed foods. If you want to avoid gluten, start by reading food labels.
As of now, fresh, unprocessed, healthy foods should be preferred above all else, as most whole foods are naturally gluten-free.

You should avoid this
- Processed food
- Cereals and grains that contain gluten. Gluten-free grains include corn, quinoa, rice, millet, buckwheat, amaranth and oats)
- However, even if oats are naturally gluten-free, they may be contaminated by gluten from the production facility. Therefore, it is safest to only use oats that are labeled gluten-free(26).
Fortunately, there are many healthy and tasty foods that are naturally gluten-free. So giving up gluten doesn’t have to be tasteless or boring.
| Contains gluten | Gluten free | |
| Wheat | Maize | Meat |
| Spelt | Quinoa | Fish / Seafood |
| Rye | Rice | Eggs |
| Barley | Millet | Dairy products |
| Bread | Buckwheat | Fruits |
| Pasta | Amaranth | Vegetables |
| Cereals | Oats | Nuts |
| Beer | Fats, oils and butter | |
| Cakes, cookies and pastries | Herbs and spices | |
It is better to avoid processed gluten-free products. These, in fact, usually have fewer nutrients and high additions of sugar or refined grains. By the way, most beverages are also gluten-free, except for beer (unless it is labeled gluten-free).
Conclusion: Should you avoid gluten?
Gluten is a controversial topic in nutrition, and one in ten Germans already avoids it partially or completely. While most people can tolerate gluten without any problems, there is a clear group that benefits from avoiding it: People with coeliac disease, gluten sensitivity or wheat allergy.
For people with coeliac disease, a strict gluten-free diet is essential to maintain the health of the intestinal mucosa and prevent nutritional deficiencies. Gluten sensitivity, on the other hand, is less clearly diagnosable, but can also cause significant symptoms. New findings even suggest that gluten sensitivity may affect not only the gut but also neurological functions.
A central component in supporting the body is to specifically compensate for the consequences of a gluten-free diet or gluten intolerance. Food supplements play an important role here by:
- Prevent or remedy nutrient deficiencies: Iron, vitamin D and B vitamins in particular are often absorbed in lower quantities if the intestinal mucosa is damaged or gluten-free foods make absorption more difficult.
- Promote intestinal health: Probiotics and fiber can help to rebalance the microbiome and support the regeneration of the intestinal mucosa.
- Reduce inflammation: Omega-3 fatty acids can have an anti-inflammatory effect and promote the healing of the intestinal mucosa, which is crucial for people with chronic complaints.
Ogaenics’ entire range of organic supplements is gluten-free and designed to support people with a wide range of needs – whether it’s by boosting gut health, providing essential micronutrients or supporting general wellbeing. So you can be sure that no hidden sources of gluten are affecting your health.
Whether you should ultimately avoid gluten depends on your individual tolerance. It is important not to switch to a gluten-free diet too quickly, but to first have medical examinations such as antibody tests and possibly a small intestine biopsy carried out to find out the cause of your symptoms.
If you decide to follow a gluten-free diet, it is important to do so consciously. A balanced diet with fresh, unprocessed foods not only helps to avoid deficiencies, but also promotes your long-term health. Living gluten-free doesn’t automatically mean being healthier – but with the right approach, you can give your body exactly what it needs to feel good.
If you want to learn more about gut health, probiotics and the microbiome, read on here:
- How menopause affects your gut health
- Skin problems? The gut-skin axis is behind it
- The crucial role of the microbiome for gut health
- Irritable bowel syndrome: Vitamin D can banish flatulence
- Get rid of flatulence: What really helps
- How the microbiome influences our health and ageing
- Bloated belly while traveling: how to prevent it
- What you should look for in a probiotic
- What can I expect when I take probiotics?
- Optimize your gut health with synbiotics
- What is turmeric actually good for?















 No products in the cart.
No products in the cart.