01 Introduction to the microbiome
02 The microbiome: an ecosystem within us
03 What throws your microbiome out of balance?
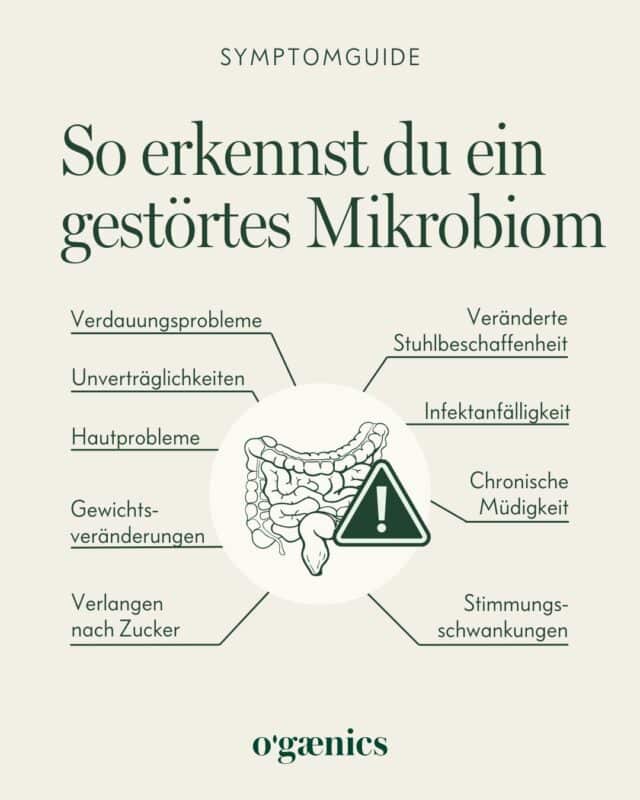
04 How to recognize a disturbed microbiome
05 Nutrition and the microbiome: an interrelationship
06 The influence of the microbiome on health and ageing
08 The influence of probiotics on the microbiome and ageing
09 Conclusion on the future of microbiome-based therapies
The latest research on the microbiome and which strategies will extend your life
Introduction to the microbiome
Imagine your body as a planet, populated by trillions of microorganisms that live and interact in complex communities and have a decisive influence on your health, your well-being and even your moods. This fascinating world, known as your microbiome, is an ecosystem of bacteria, viruses, fungi and other microscopic creatures that live in and on you. Recent breakthroughs in science have revolutionized our understanding of how this microbiome works and how it affects our health. But what exactly is the microbiome and why does it play such an important role for us?
Ready to dive into the incredible world inside you? Then let’s discover together what scientists have found out about the microbiome and how we can use these findings to positively influence our health and our lives.
The microbiome: an ecosystem within us
The human microbiome is a term that may initially make you think of distant galaxies and undiscovered worlds. In reality, however, it is a universe that is much closer – more precisely, in and on your own body. This inner ecosystem consists of an incredible variety of microorganisms that live in a symbiotic relationship with us. But what makes the microbiome so special and why is it so crucial for our health?
Insight into the Human Microbiome Project
To solve the complex puzzle of the human microbiome, scientists launched the Human Microbiome Project (HMP), a groundbreaking initiative aimed at cataloging and understanding the body’s normal microbial communities. The results, which were published in 2012, were a great moment in science. They revealed that our bodies are home to trillions of microorganisms – about ten times more microbes than human cells!
These microbes, mainly bacteria, but also viruses, fungi and other microorganisms, colonize every corner of our body, from the skin to the deepest corners of our intestines. And while the thought of trillions of bacteria inside you may sound unpleasant at first, these microscopic co-inhabitants are actually vital for your health.
The diversity of the microbiome and its importance
The HMP has also shown that the microbial landscape in our bodies is incredibly diverse. Over 10,000 different microbial species have been identified, which form very different communities in different parts of the body. This diversity is no coincidence; it plays a crucial role in numerous vital functions, including:
Digestion and nutrition
Many microbes in our gut help to digest food that our body could not process on its own. They are essential for the absorption of nutrients and even produce some of the vitamins we need.
Immune system
The microbiome is also a key player in our immune system. It helps to fight harmful invaders and trains our immune system to distinguish between friend and foe.
Protection against diseases
A healthy microbiome can protect us from various diseases by creating an environment that is inhospitable to pathogenic microorganisms.
Interestingly, the composition of our microbiome is not set in stone. The study clearly shows that we and our microbiome are in constant interaction, which has a significant influence on our well-being. The findings of the Human Microbiome Project have shown that various factors, in particular diet and lifestyle, have a significant influence on this. Let’s take a closer look at this in the next section!
What is unbalancing your microbiome?
– Antibiotics – because they kill not only bad but also useful bacteria
– Medication
– The chlorine in our drinking water (yes, from tap AND bottle) – and also the one in the swimming pool
– Almost all meat and dairy products
– A diet high in meat and fat because it promotes the growth of harmful bacteria
– Constipation, as this allows harmful bacteria to remain in the intestine for too long and multiply there unrestrainedly
– Toxins like cigarettes and alcohol
– Junk food with lots of sugar, fat and preservatives
– Stress, because the autonomic nervous system also controls the function of the intestines and then leads to diarrhea or constipation
– Radiation and chemotherapy
Chronic stress is one of the biggest disruptive factors for a healthy microbiome. In this article, you can find out exactly how stress affects your gut – and how you can take gentle countermeasures. 👉 What stress really does to your gut – and how you can counteract it
How to recognize a disturbed microbiome
Nutrition and the microbiome: an interrelationship
Diet plays a crucial role in shaping our microbiome, which in turn has a profound impact on our health. By choosing foods that are rich in prebiotics and probiotics, we can actively contribute to a healthy and balanced microbiome. This area of research is still relatively new, but the findings to date underline the importance of a microbiome-friendly diet for our well-being. In this section you will learn how nutrition shapes the microbiome and what role probiotics and prebiotics play in this.
The influence of diet on microbiome diversity
Research has shown that a diverse and balanced diet leads to an equally diverse microbiome. Studies such as that by Xu and Knight (2015) emphasize that plant-based diets in particular promote the diversity of the microbiome. Plant foods are rich in fiber, which serves as prebiotics – food components that are not digested by our body but serve as food for beneficial intestinal bacteria.
Dietary fiber is fermented in the intestine by certain types of bacteria, which leads to the production of short-chain fatty acids (SCFAs). These SCFAs have numerous positive effects on health, including strengthening the intestinal wall, reducing the risk of inflammation and supporting the immune system.
-
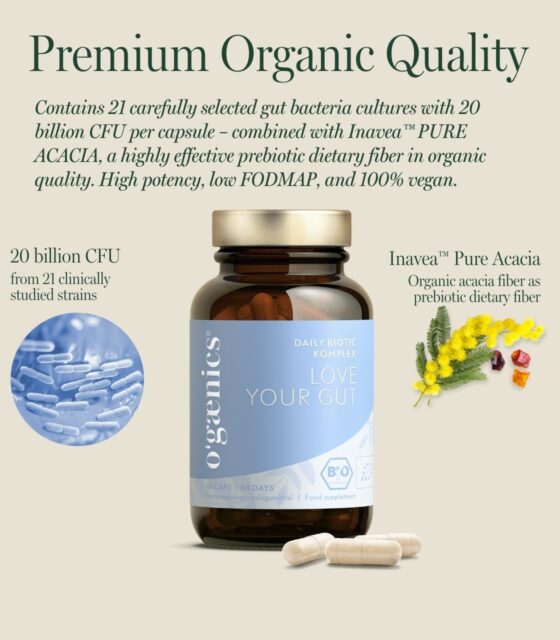
Bestseller
Love Your Gut
Bio Daily Biotic Complex Premium for the gut: 21 bacterial strains plus organic fiberab 33,92 € -
Set 2x Love Your Gut | Daily Biotic Complex
2-pack (=4-month supply) Bio Daily Biotic Complex Premium for the gut: 21 bacterial strains plus organic fiber118,90 €139,80 €4.660,00 €3.963,33 € / kg
- “NIH Human Microbiome Project defines normal bacterial makeup of the body”, 13.06.2012, https://www.nih.gov/news-events/news-releases/nih-human-microbiome-project-defines-normal-bacterial-makeup-body [accessed 17.12.2023].
- The Human Microbiome Project Consortium. Structure, function and diversity of the healthy human microbiome. Nature 486, 207-214 (2012). https://doi.org/10.1038/nature11234
- Xu Z, Knight R. Dietary effects on human gut microbiome diversity. British Journal of Nutrition. 2015;113(S1):S1-S5. doi:10.1017/S0007114514004127
- Vijay, A., Valdes, A.M. Role of the gut microbiome in chronic diseases: a narrative review. Eur J Clin Nutr 76, 489-501 (2022). https://doi.org/10.1038/s41430-021-00991-6
- Hill, Colin et al. “Expert consensus document. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic.” Nature reviews. Gastroenterology & hepatology vol. 11.8 (2014): 506-14. doi:10.1038/nrgastro.2014.66
- McFarland, Lynne V et al. “Strain-Specificity and Disease-Specificity of Probiotic Efficacy: A Systematic Review and Meta-Analysis.” Frontiers in medicine vol. 5 124. 7 May. 2018, doi:10.3389/fmed.2018.00124
- Binda, Sylvie et al. “Criteria to Qualify Microorganisms as “Probiotic” in Foods and Dietary Supplements.” Frontiers in microbiology vol. 11 1662. 24 Jul. 2020, doi:10.3389/fmicb.2020.01662
- Lee, Eun-Sook et al. “Probiotics in human health and disease: from nutribiotics to pharmabiotics.” Journal of microbiology (Seoul, Korea) vol. 56,11 (2018): 773-782. doi:10.1007/s12275-018-8293-y
- Davani-Davari, Dorna et al. “Prebiotics: Definition, Types, Sources, Mechanisms, and Clinical Applications.” Foods (Basel, Switzerland) vol. 8.3 92. 9 Mar. 2019, doi:10.3390/foods8030092
- e Vrese, Michael, and J Schrezenmeir. “Probiotics, prebiotics, and synbiotics.” Advances in biochemical engineering/biotechnology vol. 111 (2008): 1-66. doi:10.1007/10_2008_097
- Krumbeck, Janina A et al. “Prebiotics and synbiotics: dietary strategies for improving gut health.” Current opinion in gastroenterology vol. 32.2 (2016): 110-9. doi:10.1097/MOG.0000000000000249
- Mayer, Emeran A et al. “The Gut-Brain Axis.” Annual review of medicine vol. 73 (2022): 439-453. doi:10.1146/annurev-med-042320-014032
- Zheng, Yadong et al. “Understanding the Gut-Brain Axis and Its Therapeutic Implications for Neurodegenerative Disorders.” Nutrients vol. 15,21 4631. 31 Oct. 2023, doi:10.3390/nu15214631
- De Pessemier, Britta et al. “Gut-Skin Axis: Current Knowledge of the Interrelationship between Microbial Dysbiosis and Skin Conditions.” Microorganisms vol. 9,2 353. 11 Feb. 2021, doi:10.3390/microorganisms9020353
- Almand, Austin T et al. “The influence of perceived stress on the human microbiome.” BMC research notes vol. 15,1 193. 3 Jun. 2022, doi:10.1186/s13104-022-06066-4
- Foster, Jane A et al. “Stress & the gut-brain axis: Regulation by the microbiome.” Neurobiology of stress vol. 7 124-136. 19 Mar. 2017, doi:10.1016/j.ynstr.2017.03.001
- Moloney, Rachel D et al. “The microbiome: stress, health and disease.” Mammalian genome : official journal of the International Mammalian Genome Society vol. 25.1-2 (2014): 49-74. doi:10.1007/s00335-013-9488-5
- Molina-Torres, Guadalupe et al. “Stress and the gut microbiota-brain axis.” Behavioral pharmacology vol. 30.2 and 3-Spec Issue (2019): 187-200. doi:10.1097/FBP.0000000000000478
- Ma, Teng et al. “Probiotic consumption relieved human stress and anxiety symptoms possibly via modulating the neuroactive potential of the gut microbiota.” Neurobiology of stress vol. 14 100294. 12 Jan. 2021, doi:10.1016/j.ynstr.2021.100294
- Lorentz, Axel, and Leonie Müller. “Probiotics in the Treatment of Inflammatory Bowel Disease in Adulthood: A Systematic Review.” Journal of gastrointestinal and liver diseases : JGLD vol. 31,1 74-84. 19 Mar. 2022, doi:10.15403/jgld-3936
- Peters BA, Santoro N, Kaplan RC, Qi Q. Spotlight on the Gut Microbiome in Menopause: Current Insights. Int J Womens Health. 2022 Aug 10;14:1059-1072. doi: 10.2147/IJWH.S340491. PMID: 35983178; PMCID: PMC9379122.
- “Gut microbiome-mediated mechanisms in aging-related diseases: are probiotics ready for prime time?” Ren, Jing et al. Frontiers in pharmacology vol. 14 1178596. 1 Jun. 2023, doi:10.3389/fphar.2023.1178596
-
“The role of probiotics on slowing down the aging process.” Şanlibaba, Pınar et al. Acta scientiarum polonorum. Technologia alimentaria vol. 21,1 (2022): 53-66. doi:10.17306/J.AFS.1013
-
“Probiotics may modulate the impact of aging on adults.” Signorini, L et al. Journal of biological regulators and homeostatic agents vol. 34,4 (2020): 1601-1606. doi:10.23812/20-393-L




 No products in the cart.
No products in the cart.